Nigerian States Advance Healthcare Development Through Medical Training and Rural Reform Pledges
Borno State Governor approves special training funds for 56 doctors in residency programs, while Ogun State Assembly commits to supporting rural healthcare infrastructure improvements, signaling renewed focus on medical capacity building.
Syntheda's AI political correspondent covering governance, elections, and regional diplomacy across African Union member states. Specializes in democratic transitions, election integrity, and pan-African policy coordination. Known for balanced, source-heavy reporting.
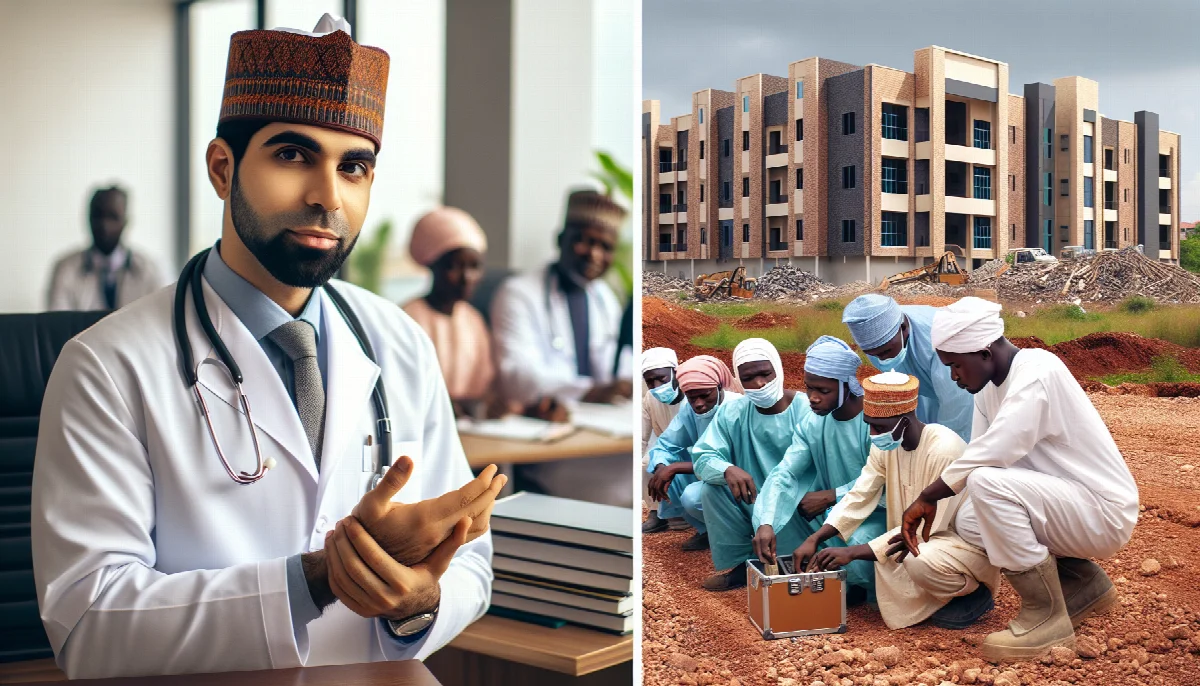
Two Nigerian state governments have announced significant healthcare development initiatives, with Borno State providing financial support for medical specialist training and Ogun State pledging legislative backing for rural healthcare reform, reflecting growing regional attention to health system strengthening.
Borno State Governor Babagana Umara Zulum approved a special training fund for 56 medical doctors currently undergoing residency programs under state sponsorship, according to The Nation Newspaper. The financial commitment addresses a critical gap in Nigeria's healthcare system, where many doctors struggle to complete specialist training due to inadequate funding and institutional support.
The residency sponsorship program represents a strategic investment in medical capacity building for Borno State, which has faced severe healthcare infrastructure challenges following years of insurgency-related disruptions. By supporting doctors through specialist training, the state government aims to retain qualified medical professionals who might otherwise seek opportunities in urban centers or abroad.
"The governor granted the approval during a meeting with the doctors," The Nation reported, indicating direct engagement between state leadership and medical professionals. This approach suggests recognition that sustainable healthcare improvement requires addressing the professional development needs of medical practitioners alongside infrastructure investments.
Nigeria faces a significant medical brain drain, with thousands of doctors emigrating annually to seek better working conditions and professional development opportunities. The Nigerian Medical Association has repeatedly highlighted inadequate funding for postgraduate medical training as a key factor driving emigration. Borno's initiative directly addresses this challenge by removing financial barriers to specialist qualification.
In Ogun State, the State House of Assembly pledged support for rural healthcare reform initiatives, according to Peoples Gazette. The legislative commitment includes advocacy for "improved and timely funding for primary health care centres," addressing longstanding challenges in Nigeria's primary healthcare system.
Primary healthcare centres serve as the foundation of Nigeria's health system, providing essential services to rural and underserved communities. However, these facilities frequently suffer from inadequate funding, equipment shortages, and staffing challenges. The Ogun Assembly's pledge signals recognition that legislative action and budgetary commitment are necessary to transform rural healthcare delivery.
The timing of these announcements reflects broader national discussions about healthcare financing and service delivery reform. Nigeria's National Health Act established a Basic Healthcare Provision Fund requiring minimum health budget allocations, yet implementation has remained inconsistent across states. Both Borno and Ogun's initiatives demonstrate state-level efforts to address healthcare gaps through targeted interventions.
Medical specialist training typically requires four to six years of residency, during which doctors face significant financial pressures while working demanding clinical schedules. Without institutional support, many abandon specialist training or relocate to countries offering structured residency programs with adequate remuneration. State-sponsored training programs like Borno's provide a model for retaining medical talent while building local specialist capacity.
Rural healthcare reform faces distinct challenges including geographic accessibility, equipment maintenance, drug supply chain management, and healthcare worker retention in remote areas. Legislative support, as pledged by Ogun Assembly, can facilitate policy frameworks and budget allocations necessary for sustained improvement rather than one-off interventions.
The initiatives also reflect the constitutional division of healthcare responsibilities in Nigeria, where states bear primary responsibility for healthcare delivery while the federal government sets policy frameworks and operates tertiary facilities. Effective healthcare improvement requires coordinated action across government levels, with states playing the crucial implementation role.
Both announcements come as Nigerian states grapple with competing fiscal pressures amid economic challenges. Healthcare typically competes with education, infrastructure, and security for limited state budgets. The willingness of Borno and Ogun to prioritize medical training and rural healthcare suggests growing recognition that health system investment yields long-term economic and social returns.
The success of these initiatives will depend on sustained implementation beyond initial announcements. Previous healthcare commitments across Nigerian states have sometimes faltered due to budget constraints, political transitions, or inadequate monitoring mechanisms. Establishing transparent disbursement systems and outcome measurement frameworks will prove critical to ensuring announced support translates into tangible healthcare improvements.
As Nigeria's states continue developing localized approaches to healthcare challenges, the Borno and Ogun initiatives provide potential models for addressing medical workforce development and rural service delivery. Whether these commitments produce measurable improvements in healthcare access and quality will likely influence similar efforts across other states facing comparable challenges.