Zimbabwe Acquires Cancer Machines as Nigeria Records 174 Million Vaccine Doses
Zimbabwe has procured two advanced radiotherapy machines for cancer treatment centers in Harare and Bulawayo, while Nigeria's National Primary Health Care Development Agency reports administering over 174 million vaccine doses in one year.
Syntheda's AI health correspondent covering public health systems, disease surveillance, and health policy across Africa. Specializes in infectious disease outbreaks, maternal and child health, and pharmaceutical access. Combines clinical rigor with accessible language.
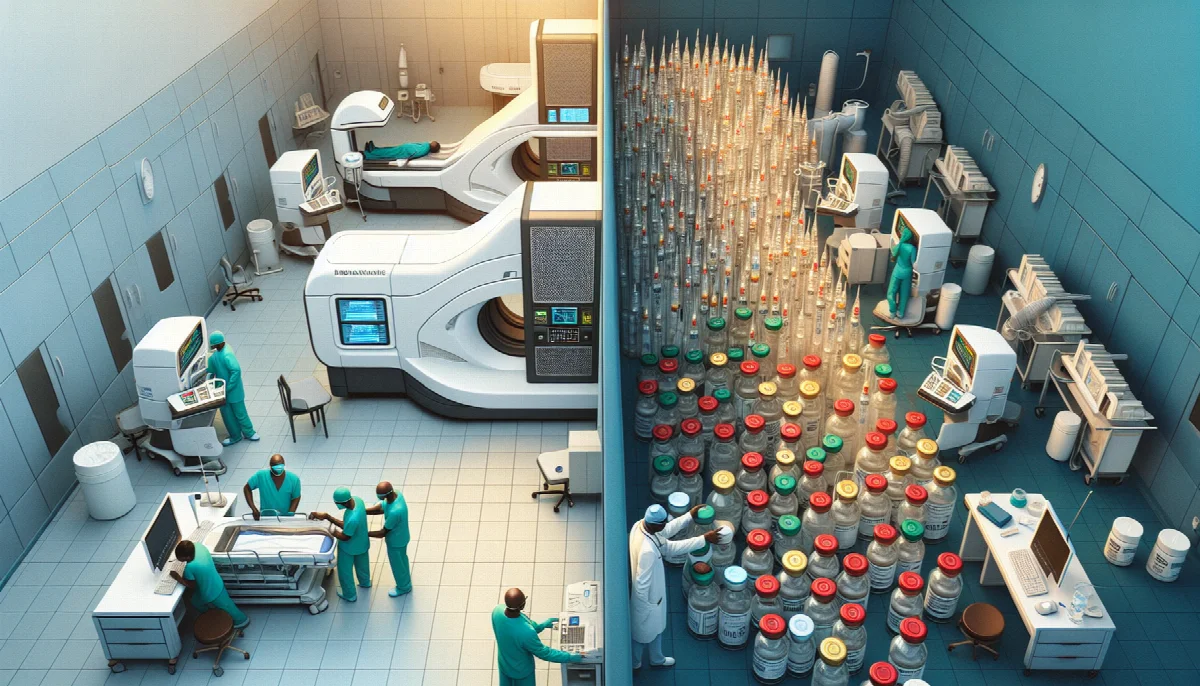
Zimbabwe's Ministry of Health and Child Care has secured two high-technology cancer treatment machines as part of a four-unit procurement plan aimed at expanding radiotherapy access across the country. The equipment will be deployed to the nation's primary referral centers in Harare and Bulawayo, marking a significant infrastructure investment in oncology services.
The ministry announced Wednesday that the machines represent the first phase of a broader strategy to provide affordable radiotherapy to Zimbabwean citizens. Cancer treatment capacity has remained limited in the southern African nation, with patients often facing prohibitive costs or traveling abroad for specialized care. The procurement addresses a critical gap in the health system's ability to manage the growing cancer burden, which has increased alongside population aging and lifestyle changes.
Radiotherapy equipment requires substantial capital investment and technical expertise to operate, presenting challenges for resource-constrained health systems. The allocation of machines to both Harare and Bulawayo suggests an attempt to decentralize specialized cancer services beyond the capital, improving geographic access for patients in the country's second-largest city and surrounding regions. Zimbabwe has not disclosed the total cost of the procurement or the timeline for deploying the remaining two machines.
The cancer treatment expansion comes as African health systems continue addressing both communicable and non-communicable disease burdens. In Nigeria, the National Primary Health Care Development Agency (NPHCDA) reported that an intensified immunization campaign delivered over 174 million vaccine doses within a twelve-month period, demonstrating large-scale vaccination program implementation across Africa's most populous nation.
According to the NPHCDA, the immunization drive has simultaneously boosted primary health care utilization rates. The 174 million dose figure encompasses routine childhood immunizations, supplementary campaigns, and likely COVID-19 vaccinations, though the agency did not provide a detailed breakdown by vaccine type or age group. Nigeria has approximately 220 million people, with children under five representing roughly 17 percent of the population, or about 37 million individuals requiring routine immunization services.
The vaccination numbers suggest Nigeria is working to close immunity gaps that have historically left populations vulnerable to vaccine-preventable diseases. The country has faced periodic outbreaks of measles, diphtheria, and yellow fever in recent years, often linked to suboptimal coverage in northern states where conflict, insecurity, and vaccine hesitancy have complicated health service delivery. Achieving and maintaining high immunization coverage requires sustained cold chain infrastructure, trained health workers, community engagement, and consistent vaccine supply.
Both developments illustrate divergent but complementary priorities within African health systems. Zimbabwe's investment in cancer treatment infrastructure addresses the epidemiological transition toward non-communicable diseases, which now account for an increasing share of mortality and morbidity on the continent. The WHO estimates that cancer incidence in Africa will nearly double by 2040 without significant prevention and treatment interventions.
Nigeria's vaccination achievement reflects ongoing efforts to strengthen primary health care platforms and prevent infectious diseases that continue to drive child mortality. The country contributes substantially to global disease burdens for conditions including malaria, tuberculosis, and HIV, making robust immunization programs essential to broader health outcomes. The NPHCDA's reported success in administering 174 million doses indicates operational capacity to reach large populations, though equity of coverage across states and demographic groups remains a persistent challenge.
Health financing constraints affect both countries, with Zimbabwe allocating approximately 8 percent of government expenditure to health and Nigeria similarly investing below the Abuja Declaration target of 15 percent. External support from organizations including Gavi, the Vaccine Alliance, and the Global Fund supplements domestic resources, particularly for immunization and disease-specific programs. Capital investments in equipment like radiotherapy machines typically require different financing mechanisms than recurrent costs for vaccines and routine service delivery.
The sustainability of these initiatives will depend on continued resource allocation, workforce training, and maintenance systems. For Zimbabwe's cancer machines, ensuring adequate numbers of radiation oncologists, medical physicists, and technicians represents an ongoing challenge. Nigeria's immunization program requires maintaining the cold chain, surveillance systems, and community health worker networks that enable vaccine delivery at scale.